 In this kind of bleedings, one of the big arteries in the base of the brain ruptures. The leaking blood spreads through the brain and into the cerebrospinal fluid.
In this kind of bleedings, one of the big arteries in the base of the brain ruptures. The leaking blood spreads through the brain and into the cerebrospinal fluid.
The reason behind most of the subarachnoid hemorrhages is the rupture of an existing aneurysm (vessel balloon) in the brain. The walls of these aneurysms are thin and so, are prone to rupture.
These aneurysms are present in some people and not present in others. The reason is unknown. Some people have aneurysms from birth but they do not rupture through a lifetime. However, the results of a ruptured aneurysm are usually very serious.
Almost half of the patients with bleeding aneurysms die. One reason other than aneurysms is arteriovenous malformations (tangle of vessels).
Who has subarachnoid hemorrhage?
Even though the incidence of brain aneurysms is 5-10% in the general population, this type of bleeding is usually observed in 1 in 10000 people. 5-10% of all strokes occur due to subarachnoid hemorrhages. They are usually seen in people aged 20-60. It is seen slightly more in females than males.
Do all subarachnoid hemorrhages occur due to ruptured arteries?
No. There is no ruptured artery in a small part of subarachnoid hemorrhages. These types of bleedings usually occur spontaneously and are usually seen in perimesencephalic spaces in the brain. The chance of healing is very high in this kind of subarachnoid hemorrhages. They are thought to occur due to veins or thin capillaries.
What are the signs and symptoms of subarachnoid hemorrhage?
The most common symptom is sudden-onset, “thunderclap” headache. Fainting and epileptic seizures usually follow this headache like a sudden blow. Patients usually describe this headache as “the worst pain experience so far”. There might be a feeling of explosion in the head before the pain. The pain, which is present in the whole head, is usually more severe in the back side. Nausea and vomiting may as well be present. Also, confusion, decreased attention and altered level of consciousness up to coma may be observed. Visual disturbances, double vision, blind spots in vision or sudden vision loss in one eye can also occur. The neck is painful and stiff. The light may disturb the eyes. There may be neck and back pain. The patient can have seizures. The patient can be unable to move or sense a part of the body. Personality disorders, confusion or aggression may be observed.
TREATMENT:
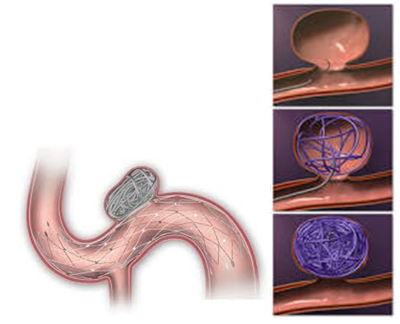
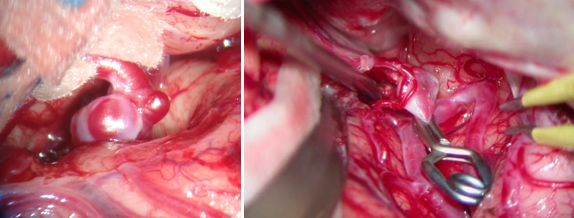
If the patient is able to reach a hospital (usually more than half of the patients who suffer from this bleeding die at the scene), the treatment starts in the intensive care unit. The aim of treatment is this: The patient had a brain hemorrhage due to a ruptured aneurysm in the brain. The bleeding stopped on its own, but the patient survived and was reached to a hospital. However, a second bleeding is only a matter of time. A second bleeding would result in the death of the patients, so the aneurysm must be closed somehow. First, the location of the aneurysm in the brain is determined with brain angiography (CT, MRI or conventional angiography from groin). Then, brain surgeons and interventional neuroradiology doctors consult to determine which technique is better, “endovascular embolization” or “direct brain surgery”, and carry on with the determined technique. Endovascular embolization is entering the vessels from the inguinal region with a very thin wire, reaching the aneurysm in the brain and filling the aneurysm with blocking material. This way, it is prevented from bleeding again. Direct brain surgery is the preferred technique when this method is unavailable for any reason (e.g, aneurysm not being suitable for this treatment). In this surgery, the skull is opened; the aneurysm is identified in the brain with a microscope and is closed with a clip to prevent re-bleeding. The next stage is the recovery of brain damage caused by the bleeding with intensive care unit treatment.